The word ‘cancer’ came from Latin word ‘cancrum’ meaning crab. It is a group of diseases characterized by uncontrolled cell division leading to the growth of abnormal tissue/ tumor. Cancer is a disease of cell in which abnormal cells containing abnormal genetic content divide without control and invade nearby tissue. Cancer cells transfer through blood and lymph. Oncology, a branch of medicine that deals with etiology, diagnosis, treatment and prevention of cancer. ‘Onco’ is a Greek word meaning tumor.
${tocify}
Types of Cancer
Carcinoma: Begins in different organs, glands, skin or tissues that cover other organs. E.g. breast cancer, colon cancer, rectal cancer etc.
Sarcoma: Cancer of supportive or connective tissues. Begins in bone, cartilage, muscle or blood vessel. E.g. bone cancer (Osteosarcoma), angiosarcoma, chondrosarcoma, liposarcoma.
Leukemia: Begins in blood forming tissue. E.g. bone marrow cancer.
Lymphoma and myeloma: are cancers of the immune system. Begins in lymphatic system.
Cancer of nervous system: E.g. brain cancer.
Teratoma: Cancer of germ cells (testis or ovary).
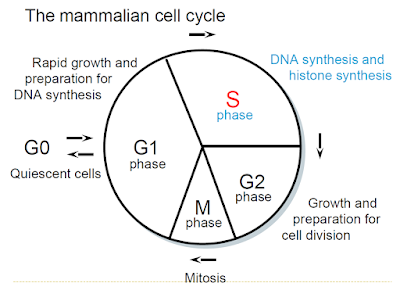
Cell Proliferation
- Normal physiologic process
- Response to injury
- Immune responses
- To replace cells that have died
- To replace cells that have been shed as a part of their life cycle (e.g. skin, mucous membrane of GI tract, etc.)
Characteristics of Cancer Cells
- Uncontrolled proliferation
- Abnormal nucleus
- Loss of anchorage - The requirement by normal cells to attach to a surface to grow and divide in vitro; when cells lose anchorage dependence they no longer respond to external growth controls, which often correlates with tumorigenicity in vivo. It is a hallmark of malignant transformation
- loss of contact inhibition- Contact inhibition enables noncancerous cells to cease proliferation and growth when they contact each other. This characteristic is lost when cells undergo malignant transformation, leading to uncontrolled proliferation and solid tumor formation.
- Forms tumor
- Undergoes metastasis & angiogenesis
- Lack of differentiation into specialized cells.
- Increased rate of anaerobic glycolysis
Difference between Normal Cell and Cancer Cell
Etiology of Cancer
- Physical (e.g. x-ray, gamma ray, UV light etc.)
- Chemical (e.g. asbestos, aflatoxins (Aspergillus flavus and Aspergillus parasiticus), aniline, nitroso compound etc.)
- Biological (viruses like Human Papilloma virus, Hepatitis B virus)
- Environmental factors (physical & chemical agents)
- Genetic
- Mutation
- Life style: tobacco smoking or chewing, alcohol
Mutation
- Sudden change in the chemical structure of the DNA
- The substance which causes mutation is known as ‘mutagen’. (e.g. x-ray, gamma ray)
Carcinogenesis
- Requires abnormal genetic content
- Requires three steps:
- Activation of proto-oncogene to oncogene
- Deregulation of tumor suppressor gene and DNA repair gene
- Immortalization
Genes Responsible for Cancer
1. Oncogene
2. Tumor suppressor gene
3. DNA repair gene
- Senescence
- Apoptosis
- Cancer
Immortalization
4. Telomerase reverse transcriptase (TERT)
- Telomerase is an enzyme that provides for telomere synthesis and maintenance, thus telomerase may potentially allow for cellular immortality.
- Telomerase activity may promote tumors through multiple, complex mechanisms, especially by subverting the normal DNA synthetic checkpoints.
Molecular Causes of Cancer
1. Abnormal karyotype:
2. Rearrangement of nucleotides:
- Within the same chromosome: homologous rearrangement
- With other chromosome: non-homologous rearrangement
3. Mutation:
- Transition: purine by purine (A by G), pyrimidine by pyrimidine (C by T)
- Transversion: purine by pyrimidine or vice-versa (A by C or C by A etc.)
4. Abnormal genetic content:
5. Activation of oncogene
6. Loss of activity of tumor suppressor gene:
7. Mutation in DNA repair gene:
8. Blocking apoptosis:
Major Approaches for Cancer Treatment
1. Destruction of neoplastic cells:
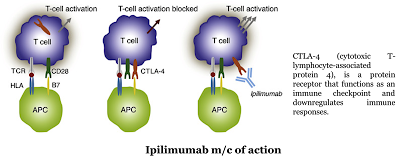
- Checkpoint modulators: Nivolumab, pembrolizumab. Immunotherapy drugs called immune checkpoint inhibitors work by blocking checkpoint proteins from binding with their partner proteins. This prevents the “off” signal from being sent, allowing the T cells to kill cancer cells.
- Therapeutic antibody: Brentuximab vedotin
2. Surgery:
3. Metastasis blocking:
4. Convert tumor cell to normal cell:
5. Halt neoplastic cell division:
6. Block angiogenesis:
Molecular Mechanism for Resistance against Anticancer Drugs
- Decreased drug uptake: To act as an anticancer drug, the drug must be uptaken by the cancer cells. So, if the cell does not uptake the anticancer drug, the drug will be resistant. E.g. Methotrexate, actinomycin D etc.
- Increased drug efflux: Phosphoglycoprotein (PGP) is over expressed and efflux of drug is increased. The drug then can not act as an anticancer drug. E.g. doxorubicin, actinomycin D etc.
- Decreased conversion to active drug: Some drugs are given as pro-drug. So, these drugs must be activated inside the body. If these drugs are not activated, they will not be able to kill cancer cells. E.g. Cyclophosphamide (inactive) is activated to active cyclophosphamide by metabolic activation.
- Increased conversion of active to inactive metabolite: To kill the cancer cells, the anticancer drug must remain in the active form. But some enzymes may convert the active drug to inactive metabolite. Thus the drug would be resistant. E.g. aldehyde dehydrogenase converts cyclophosphamide to inactive metabolites.
- Rapid repair of DNA damage: Some anticancer drugs kill the cancer cells by damaging the DNA. If the damaged DNA is repaired quickly, the drug will be resistant. E.g. cyclophosphamide, doxorubicin, etc.
- Increased intracellular concentration of the target enzyme: 5-FU inhibits thymidylate synthase. If thymidylate synthase concentration is increased, 5-FU will be resistant.
- Increased expression of apoptosis blocking protein: BCL2 blocks apoptosis. Some drugs that induce apoptosis get resistant due to over expression of BCL2.
- Presence of altered enzyme that is enzymatically active but has lower binding affinity for the drug: Methotrexate binds with DHFR. Altered DHFR does not bind to methotrexate but has normal function.
Targeted Cancer Therapy
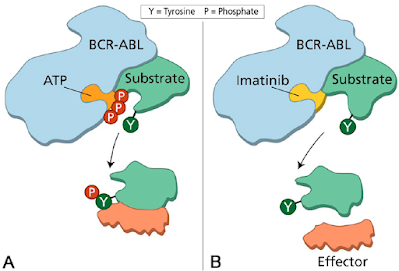
- Small molecules that can enter into the cell e.g. imatinib
- Monoclonal antibody that carry drug to the cell surface e.g. trastuzumab binds to HER-2 (Human Epidermal Growth Factor Receptor-2, inhibit the PI3K/Akt pathway and the MAPK pathway. The HER2 pathway promotes cell growth and division when it is functioning normally; however, when it is overexpressed, cell growth accelerates beyond its normal limits.).
Available Targeted Therapy
- Hormone therapy: Any drug that is used to block the action of a hormone in a hormone sensitive cancer. e.g. Tamoxifen is used to block the activity of estrogen in ER positive breast cancer.
- Signal transduction inhibitor: Once a cell receives a signal to grow, it is relayed within the cell through a process of biochemical reaction. Imatinib mesylate (tyrosine kinase inhibitor) inhibits the signal transduction of BCR-ABL fusion gene (chronic myeloid leukemia).
- Gene expression modulator: TFO (triplex forming oligonucleotide) are used to repair DNA damage. They are not very useful due to lack of specificity.
- Apoptosis inducer: If any drug can induce apoptosis in mutated cell, then carcinogenesis can be prevented. No such drug is available at the market.
- Angiogenesis inhibitor: New blood vessel production is blocked. E.g. Bevacizumab inhibits VEGF to bind with its receptor, VEGF receptor 2.
Cancer cells are cells that have lost their ability to divide in a controlled fashion. A malignant tumor consists of a population of rapidly dividing and growing cancer cells that progressively accrues mutations. However, tumors need a dedicated blood supply to provide the oxygen and other essential nutrients they require in order to grow beyond a certain size. Tumors induce blood vessel growth (angiogenesis) by secreting various growth factors (e.g. VEGF) and proteins.
Growth factors such as bFGF and VEGF can induce capillary growth into the tumor, which some researchers suspect, supply required nutrients, allowing for tumor expansion. Unlike normal blood vessels, tumor blood vessels are dilated with an irregular shape. - Immunotherapy: Drug that trigger host immune system can halt carcinogenesis. Eg: Ipilimumab is a monoclonal antibody medication that works to activate the immune system by targeting CTLA-4, a protein receptor that downregulates the immune system. Cancer cells produce antigens, which the immune system can use to identify them. These antigens are recognized by dendritic cells that present the antigens to cytotoxic T lymphocytes (CTLs) in the lymph nodes. The CTLs recognize the cancer cells by those antigens and destroy them. However, along with the antigens, the dendritic cells present an inhibitory signal. That signal binds to a receptor, cytotoxic T lymphocyte-associated antigen 4 (CTLA-4), on the CTL and turns off the cytotoxic reaction. This allows the cancer cells to survive. Ipilimumab binds to CTLA-4, blocking the inhibitory signal, which allows the CTLs to destroy the cancer cells.
- Monoclonal antibodies that deliver toxic molecules: Toxic materials attached to monoclonal antibody can specifically bind to and release toxic substance into the cancer cells. For example, ibritumomab tiuxetan can bind to CD20 and destroy cancer cell by releasing radioactive isotope attached to it. The drug uses the monoclonal mouse IgG1 antibody ibritumomab in conjunction with the chelator tiuxetan, to which a radioactive isotope (either yttrium-90 or indium-111) is added.